
Advancing women’s health: bridging the gender gap using the BIOMATDB tools
Gender imbalances in medical research can lead to less effective treatments for women. Biomaterials databases and marketplaces can bridge this gap, promoting better health for all.
Gender disparities in biomedical research often result in medical treatments that fail to address the needs of women adequately. This
issue is also relevant for the development of biomaterials. Innovative tools like the BIOMATDB biomaterials database and marketplace are being developed to help ensure gender equality and diversity are included in research, leading to more inclusive and effective healthcare solutions for everyone.
Gender imbalances can significantly influence the outcomes of research and medical treatments, often making them less effective for one sex. This issue is especially critical in the field of biomaterials, where the effects of such imbalances can impact everything from laboratory research to clinical applications. However, even tools like the BIOMATDB biomaterials database and marketplace can offer promising solutions to address these disparities. Taking into consideration gender-related parameters in the research on these tools can improve inclusion and enhance health outcomes for women.
The gender gap in biomedical research
Historically, biomedical research has been dominated by men, guiding the research priorities and leading to a neglect of diseases that predominantly affect women and leaving women’s health issues underexplored. This bias has predominately favoured clinical trials being finetuned in men. However, emerging studies are sometimes breaking gender stereotypes – one such example would be osteoporosis. Despite the significant impact on older men, osteoporosis is often perceived as a “woman’s” disease, leading to even higher rates of underdiagnosis and undertreatment in male versus female patients. A 2024 study estimated that globally, one in five men over the age of 50 will experience an osteoporotic fracture in their remaining lifetime [1]. Additionally, the number of hip fractures in men is projected to increase by approximately 310% between 1990 and 2050.
Women’s bodies were often considered too complex to study due to hormonal variations, and medical intervention during pregnancy was avoided due to perceived risks to both mother and foetus, further hampering research in women’s health. The lack of understanding of female physiology and pathology includes diseases of female-specific organs, such as endometriosis and uterine cancers, diseases that disproportionately affect women, such as autoimmune disorders, and conditions that present differently in women, such as cardiovascular disease. Additionally, some women experience health problems during pregnancy. These complications can affect the health of the mother, the foetus, or both. Even women who were healthy before becoming pregnant can encounter issues that make the pregnancy high-risk. These complications include, but are not limited to, high blood pressure, gestational diabetes, infections, and preeclampsia. They can lead to adverse pregnancy outcomes such as preterm labour, pregnancy loss/miscarriage, and stillbirth. Moreover, the mother could suffer from mental health problems such as depression and anxiety, during the pregnancy and after giving birth. Thus, there is a clear need for novel biomaterial-based approaches for preventive and therapeutic applications targeting women’s health, and during pregnancy.
Notably, female inventors are more likely to address women’s health problems [2] but the lack of female representation in patent applications and more generally in science, technology, engineering, and mathematics (STEM) fields has hindered the development of solutions. Despite women making up over half of the world’s population, nearly 75% of US funding for gender-specific disorders favours men [3,4] and a 2020 McKinsey report found that only about 1% of global healthcare research and innovation is invested in female-specific conditions beyond cancer [5]. Moreover, it has been estimated that only 3.7% of clinical trials from 2007 to 2020 focused on gynaecology [6]. These disparities underline both preclinical and clinical research challenges in women’s health and hamper the development of relevant diagnostic criteria and effective treatments specifically for women.
The importance of gender equality and diversity in research
These facts and numbers are deeply concerning and there is growing recognition that women’s health has been inadequately studied and managed. A 2024 report from the World Economic Forum, in collaboration with the McKinsey Health Institute, states that the “women’s health gap” (defined as “health conditions that affect women uniquely, differently or disproportionately and lead to women spending more time in poor health”) is equivalent to 75 million years of women’s life lost due to poor health or early death each year. They estimate that closing this gap would benefit 3.9 billion women, giving them an extra seven healthy days a year, or an average of 500 days over a lifetime [7].
This is where gender equality and diversity come into play. Promoting gender equality in scientific research is not just about fairness. Increasing the ratio of female researchers enhances research perspectives, helps generating novel research questions and methods, and accelerates the development and effectiveness of treatments for women. Increasing female representation in science could speed up improvements in healthcare and facilitate wider application of research findings.
On the other hand, gender diversity also improves the quality and applicability of medical treatments for women. Male-centric approaches have shown their limits, with women twice as likely as men to experience adverse events from drugs [8]. Including both sexes in preclinical studies and clinical trials helps identify sex-specific responses as well as potential sex-specific side effects, leading to better tailored and more effective therapies.
This methodology is particularly important in developing biomaterials that have to work well in both female and male bodies despite the fact that sex differences can influence how these materials behave in the body. In fact, women and men can have different morphologies, immune responses, hormonal interactions, and healing processes. It is therefore crucial to take these differences into account when designing biomaterials, implants, prosthetics, or drug delivery systems. An example is the design of cardiovascular stents. Research has shown that women often have smaller coronary arteries and different patterns of artery disease compared to men [9]. Without considering these differences, stents might not perform as well in female patients, leading to higher rates of complications and re-interventions. Another instance of inadequate male-centred design is that of hip implants, which do not account for potential physiological differences in load bearing and therefore are more than twice as likely to fail in women [10].
Advancements in biomaterials research for women’s health
In spite of these shortcomings, recent advancements in biomaterials research hold the promise of innovative solutions that could revolutionise the diagnosis, treatment, and management of gender-specific health conditions.
One area of significant advancement lies in the development of biomaterials for reproductive health, including contraception, fertility treatments, and reproductive tissue engineering. For example, polymers such as polylactic acid (PLA), poly(ortho esters) POE) and poly-(ε-caprolactone) (PCL) are being explored as biodegradable drug delivery vehicles for long-acting contraceptive implants, to offer women a convenient and highly effective form of birth control [11]. Additionally, tissue engineering approaches utilising biomaterial scaffolds hold promise for regenerating damaged or substituting surgically removed reproductive organs, such as the uterus or ovaries. These include 3D printing using porous gelatine hydrogels [12] as well as artificial human ovary reconstruction based on hydrogels such as fibrin, alginate, or poly(ethylene) glycol (PEG) [13,14].
Breast cancer is the most common cancer worldwide, and approximately 99% of breast cancer cases occur in women [15]. Mastectomy remains a primary treatment for breast cancer patients, however the procedure can cause pain as well as emotional and psychological damage. Breast reconstruction approaches include the use of implants or autologous techniques (using one’s own body tissue to reconstruct the breast), but both present advantages and risks and fail to recreate an identical breast and fully restore the femininity of affected patients. Advances in tissue engineering approaches that utilise decellularized matrices, dermal grafts and bio-printed scaffolds are providing potentially new avenues to enabling more natural and aesthetically pleasing breast reconstruction options for women who have undergone mastectomy, restoring both physical appearance and emotional wellbeing [16,17,18].
Biomaterials have also been leveraged to address pelvic floor disorders such as pelvic organ prolapse (POP). However, polypropylene meshes were designed after those used in hernia surgeries and not for the unique physiology of the female pelvis. This led to high complication rates and therefore, their use for transvaginal surgery for pelvic organ prolapse was restricted or banned in several countries [19]. To address the issues encountered with the synthetic meshes, current studies are looking at tissue-derived mesh alternatives and novel mesh design to improve treatment options, minimise side effects, and optimise health outcomes for women suffering from POP [20,21,22].
By continuing to support and invest in research and innovation for women’s health, we can ensure that women receive the care and support they need to lead healthier, happier lives.
How the BIOMATDB biomaterials database and marketplace can help
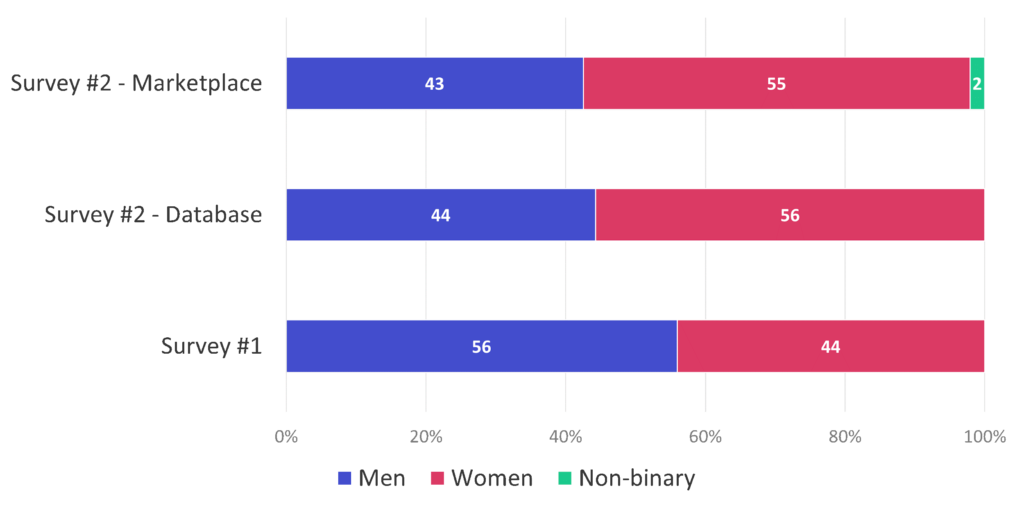
The BIOMATDB consortium strives to support gender diversity in medical research and healthcare outcomes. It actively sought to incorporate the perspectives of women stakeholders when reaching out to the biomaterials community through surveys and interviews. Indeed, thanks to targeted efforts by the consortium partners, the participation rate of women increased from 44% (D2.2 Stakeholder Survey: average of responders to the first BIOMATDB survey across categories of stakeholders who disclosed gender information) to 55.5% (D2.4 Updated Stakeholder Survey: average of responders to the second BIOMATDB surveys for either the database or marketplace across categories of stakeholders who disclosed gender information) between the two iterations of the BIOMATDB surveys (see Figure 1). Engaging with the female biomaterials community enables us to gather insights into the specific challenges and needs women face in the healthcare landscape. This inclusive approach ensures that the BIOMATDB solutions are also tailored to address the unique requirements and needs of women. Such feedback is useful to inform the solutions’ design, making them a more effective tool for identifying and developing biomaterials that are adapted to sex-specific health issues, ultimately contributing to more equitable and effective medical solutions.
The BIOMATDB database can play a role in reducing gender imbalance by providing its relevant users (such as researchers, clinicians, and product developers) with updated and relevant information on raw biomaterials and medical devices used in women’s health applications, enabling to easily search for sex-specific data on how different biomaterials or medical devices perform in male and female bodies. The approach focuses on filtering collected data to highlight gender-specific biocompatibility tests and outcomes. The innovative design of the database aims to include a comprehensive list of materials, biocompatibility tests, results, literature references, and regulatory statuses. This will help identify literature gaps crucial for all preclinical stages of development or cohorts participating in clinical trials in women’s health. Data entry will be standardised, offering search options for female versus male data, and automated tools will be used for efficient data extraction. The user interface could be tailored to feature search options and functions, subsequent filters, and visualisation tools to specifically explore biomaterials used in reproductive tissue studies, female prevalent types of pathology and possibly venture into hypothesis driven exploration of women’s health data. Backend manual curation and annotation efforts could safeguard vast data volumes and ideally future updates, finetuning and quality control measures will ensure data accuracy and reliability, with access controls to ensure access to information.
Gaps in understanding biocompatibility and toxicity in women stemming from clinical trials that were historically focused on healthy young men have highlighted the need for more inclusive trials that gather comprehensive data on women. This should be investigated using targeted approaches, as materials and devices may perform differently due to hormonal, anatomical, and physiological differences. Aiming to disentangle these confounding factors and literature gaps, the BIOMATDB database could enhance biomaterial selection and provide insight on safety in medical applications for women. The envisaged features described here would facilitate the identification of relevant evidence where sex-specific information such as adverse effect, immune response, material properties, etc. are used to ensure these sex differences are not overlooked but rather integrated in the product development process, guiding the design of more inclusive biomaterials and medical devices.
Additionally, the BIOMATDB marketplace offers lay language formatted text combined with advanced search capabilities and user-friendly interfaces. This informs researchers, patients, and clinicians about the use and variability of relevant biomaterials and medical devices that have been tested and validated for both sexes, or in women specifically, thereby encouraging the development and use of medical devices and treatments that are effective for women and providing a valuable tool for clinical decision-making. An important relevant scenario on the marketplace will be that for gynaecology (see Figure 2), which will enable to easily search for those biomaterials and medical devices that have been approved for use in this medical application. It will therefore enable women patients to get access to and read about the existing and available medical devices, supporting them in their health self-education and empowering them to make informed decisions about their health.
Conclusion
Incorporating gender perspectives in biomedical research is a fundamental step toward achieving health equity. It ensures that medical treatments are not only effective but also fair and inclusive. By addressing gender imbalances in biomaterials research and clinical practices, and utilising tools like the BIOMATDB biomaterials database and marketplace, we can move towards a future where literature gaps are filled, market needs are identified, and healthcare solutions are designed to meet the needs of all individuals.
Moreover, and beyond inclusive gender approaches, as scientists we also seek to predict, identify and avoid biomaterials adverse
effects that could be detrimental for the mother-foetus dyad and lead to adverse pregnancy outcomes. This anthropocentric side of the web tools can significantly enhance decision-making for stakeholders and clinicians alike.
Authors: Clémence Foltz, Athina Samara, Nicole Ticchi
References
- Fuggle, N.R., Beaudart, C., Bruyère, O., Abrahamsen, B., Al-Daghri, N., Burlet, N., Chandran, M., Rosa, M.M., Cortet, B., Demonceau, C., Dere, W., Halbout, P., Hiligsmann, M., Kanis, J.A., Kaufman, J.-M., Kurth, A., Lamy, O., Laslop, A., Maggi, S. and Matijevic, R. (2024). Evidence-Based Guideline for the management of osteoporosis in men. Nature Reviews Rheumatology, [online] 20(4), pp.241–251. doi: https://doi.org/10.1038/s41584-024-01094-9.
- Koning, R., Samila, S. and Ferguson, J.-P. (2021). Who do we invent for? Patents by women focus more on women’s health, but few women get to invent. Science, 372(6548), pp.1345–1348. doi: https://doi.org/10.1126/science.aba6990.
- Mirin, A.A. (2020). Gender Disparity in the Funding of Diseases by the U.S. National Institutes of Health. Journal of Women’s Health (2002), [online] 30(7). doi:https://doi.org/10.1089/jwh.2020.8682.
- Smith, K. (2023). Women’s health research lacks funding – these charts show how. [online] www.nature.com. Available at: https://www.nature.com/immersive/d41586-023-01475-2/index.html.
- www.mckinsey.com. (n.d.). Unlocking opportunities in women’s healthcare | McKinsey. [online] Available at: https://www.mckinsey.com/industries/healthcare/our-insights/unlocking-opportunities-in-womens-healthcare.
- Steinberg, J.R., Magnani, C.J., Turner, B.E., Weeks, B.T., Young, A.M.P., Lu, C.F., Zhang, N., Richardson, M.T., Fitzgerald, A.C., Mekonnen, Z., Redman, T., Adetunji, M., Martin, S.A., Anderson, J.N., Chan, K.S. and Milad, M.P. (2022). Early Discontinuation, Results Reporting, and Publication of Gynecology Clinical Trials From 2007 to 2020. Obstetrics & Gynecology, [online] 139(5), p.821. doi: https://doi.org/10.1097/AOG.0000000000004735.
- Weforum.org. (2024). World Economic Forum | Closing the Women’s Health Gap: A $1 Trillion Opportunity to Improve Lives and Economies. [online] Available at: https://www3.weforum.org/docs/WEF_Closing_the_Women.
- Zucker, I. and Prendergast, B.J. (2020). Sex differences in pharmacokinetics predict adverse drug reactions in women. Biology of Sex Differences, [online] 11(1). Available at: https://bsd.biomedcentral.com/articles/10.1186/s13293-020-00308-5.
- Taqueti, V.R. (2018). Sex Differences in the Coronary System. Advances in Experimental Medicine and Biology, pp.257–278. doi: https://doi.org/10.1007/978-3-319-77932-4_17.
- Hutchison, K. (2019). Gender Bias in Medical Implant Design and Use: A Type of Moral Aggregation Problem? Hypatia, 34(3), pp.570–591. doi: https://doi.org/10.1111/hypa.12483.
- Yan, M., Zhang, Y., Wu, Z., Li, Y., Dou, K., Wang, B., Wang, Y. and Zhou, Q. (2022). Recent progress in advanced biomaterials for long-acting reversible contraception. Journal of Nanobiotechnology, 20(1). doi: https://doi.org/10.1186/s12951-022-01329-5.
- Laronda, M.M., Rutz, A.L., Xiao, S., Whelan, K.A., Duncan, F.E., Roth, E.W., Woodruff, T.K. and Shah, R.N. (2017). A bioprosthetic ovary created using 3D printed microporous scaffolds restores ovarian function in sterilized mice. Nature Communications, [online] 8(1), p.15261. doi: https://doi.org/10.1038/ncomms15261.
- Salama, M. and Woodruff, T.K. (2019). From bench to bedside: Current developments and future possibilities of artificial human ovary to restore fertility. Acta Obstetricia et Gynecologica Scandinavica, 98(5), pp.659–664. doi: https://doi.org/10.1111/aogs.13552.
- Kinnear, H.M., Tomaszewski, C.E., Chang, F.L., Moravek, M.B., Xu, M., Padmanabhan, V. and Shikanov, A. (2020). The ovarian stroma as a new frontier. Reproduction, [online] 160(3), pp.R25–R39. doi: https://doi.org/10.1530/REP-19-0501.
- World Health Organization (2024). Breast cancer. [online] World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/breast-cancer.
- Caronna, V.C., Rosenberg, A.F., Graham, D.M., Heim, W.M., Grasperge, B.F., Sullivan, S.K., Chaffin, A.E., Bunnell, B.A. and Pashos, N.C. (2021). Viability of acellular biologic graft for nipple-areolar complex reconstruction in a non-human primate model. Scientific reports, 11(1). doi: https://doi.org/10.1038/s41598-021-94155-y.
- Sarah Van Belleghem, Bhushan Mahadik, Snodderly, K., Mote, Z., Jiang, B., Yu, J., Shannon Theresa McLoughlin, He, X., Nam, A.J. and Fisher, J.P. (2021). Dual Extrusion Patterning Drives Tissue Development Aesthetics and Shape Retention in 3D Printed Nipple‐Areola Constructs. Advanced Healthcare Materials, 10(23). doi: https://doi.org/10.1002/adhm.202101249.
- Yanis Berkane, Haizam Oubari, Loïc van Dieren, Charlès, L., Lupon, E., McCarthy, M., Cetrulo, C.L., Bertheuil, N., Uygun, B.E., Smadja, D.M. and Lellouch, A.G. (2024). Tissue engineering strategies for breast reconstruction: a literature review of current advances and future directions. Annals of Translational Medicine, [online] 12(1), pp.15–15. doi: https://doi.org/10.21037/atm-23-1724.
- Ng-Stollmann, N., Fünfgeld, C., Gabriel, B. and Niesel, A. (2020). The international discussion and the new regulations concerning transvaginal mesh implants in pelvic organ prolapse surgery. International Urogynecology Journal, 31(10), pp.1997–2002. doi: https://doi.org/10.1007/s00192-020-04407-0.
- Liang, R., Knight, K., Abramowitch, S. and Moalli, P.A. (2016). Exploring the basic science of prolapse meshes. Current Opinion in Obstetrics & Gynecology, 28(5), pp.413–419. doi: https://doi.org/10.1097/gco.0000000000000313.
- Knight, K., King, G.E., Palcsey, S., Artsen, A.M., Abramowitch, S.D. and Moalli, P. (2022). A soft elastomer alternative to polypropylene for pelvic organ prolapse repair: a preliminary study. International Urogynecology Journal, 33(2), pp.327–335. doi: https://doi.org/10.1007/s00192-021-04792-0.
- Knight, K., King, G.E., Palcsey, S., Artsen, A.M., Abramowitch, S.D. and Moalli, P. (2022). A soft elastomer alternative to polypropylene for pelvic organ prolapse repair: a preliminary study. International Urogynecology Journal, 33(2), pp.327–335. doi: https://doi.org/10.1007/s00192-021-04792-0.
Keywords
Gender equality, gender diversity, women’s health